I'm on an operating table right now, probably.
Mon, Nov 3, 10:13 AM
I am writing to you on the evening preceding an early morning surgery.
At the present time, I'm well. Pleased, satiated, happy. Hopeful. Excited for life on the other side of the operating table and thankful for the events that have brought me here.
For the past three surgeries I've had, I've taken the opportunity to leverage modern technology and schedule-send emails to be delivered while I'm blacked out and intubated on an operating table. Most of you probably haven't received one of those purgatory emails, but I thought it would be fun to make this mass email one of those. So presumably, when this is delivered to you Monday morning, I will be undergoing internal modifications.
A recap: Read the prior notices if you want. I think we last left off sometime around April when they did the previous lung surgery.
Short story: Some time ago, these nodules popped up in my lungs. It's a common spot for this cancer to spread to; the liver usually first and then the lung. They stuck a needle in my lung, looked at the contents of it under a microscope, and confirmed it's cancer.
So I did some chemo. Different cocktails of drugs that at this time I forget due to irreverence and not forgetfulness. The chemotherapies didn't shrink the lung tumors/lesions/nodules/whatever you want to call them.
As a small insight into the world of cancer doctors (and I generally really like my oncologist), there was a time when these nodules first showed up and she said they were too small to do anything with. I disagreed with that sentiment...I thought we could shoot them with radiation when they were a few mm in size. She said they were too small.
Some time and some chemo later, they had gotten bigger, and I told her we needed to do something about it. She suggested they were too big to treat. Kind of humorous. But I lobbied for mechanical intervention, and she presented my case to their board of cancer doctors. The radiation people said it was too risky and didn't love the treatment approach. The surgeon was all on board, though.
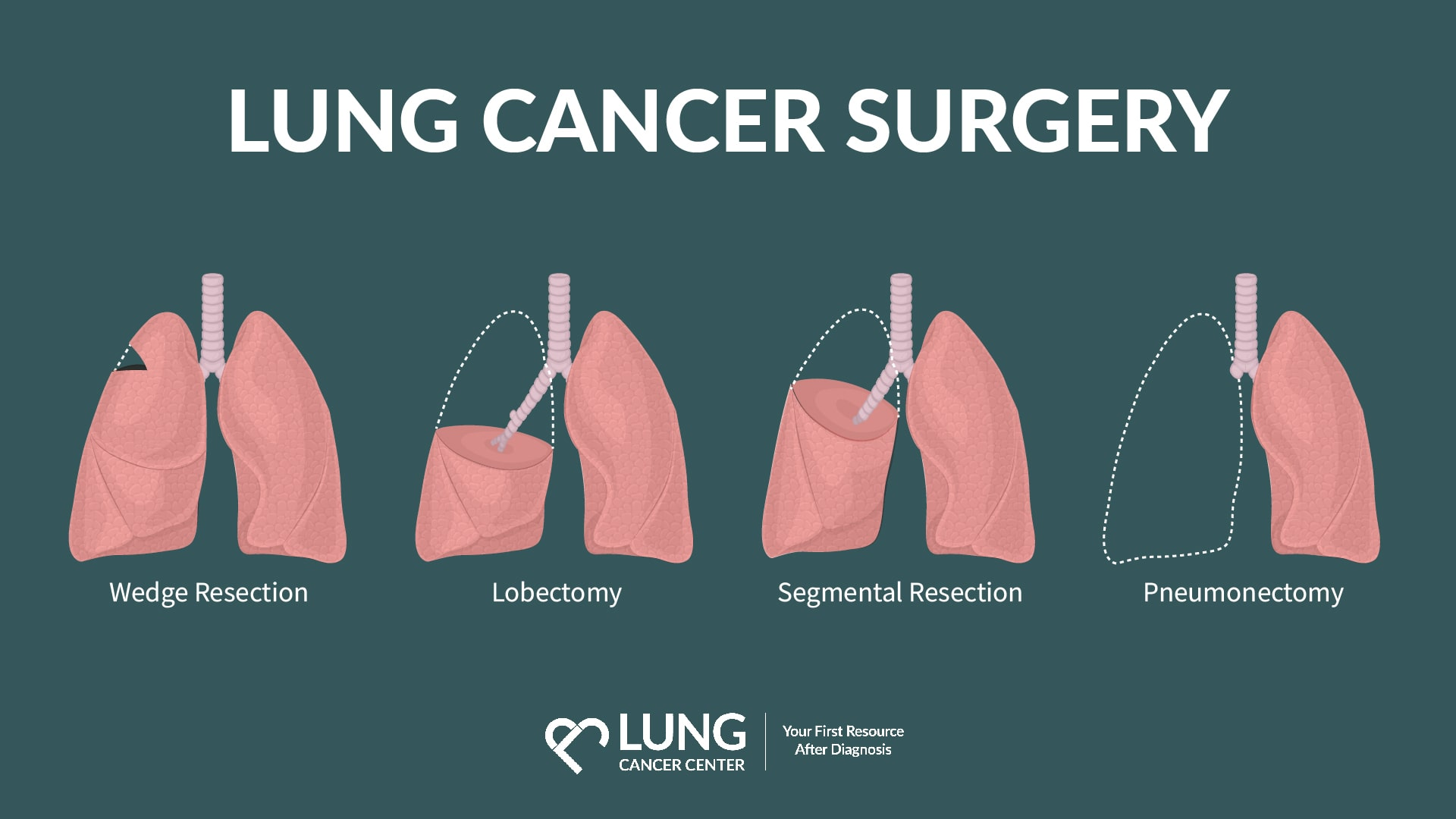
So, on April 2nd, he went to remove the upper lobe of my right lung (that lung has 3 lobes), but instead of taking the whole lobe, he just took the bad chunk out. When he was trying to remove the lobe, he found that the lung was pretty stuck to the pulmonary artery. He said that happens after chemo sometimes. So instead of removing the whole lobe, he did a wedge resection.
I was in the hospital for, I think, 20 hours after the surgery. I woke from anesthesia, they wheeled me to a room, I hung out for a bit while they monitored vitals and such, they watched my lung to make sure it didn't collapse, they eventually pulled a giant tube out of my ribcage (chest tube. Google it, it's cool) and then I walked out. The nurses and staff absolutely hate it when you walk out, so I make a point to do it. They want to call the wheelchair people and roll you out.... Ridiculous. I had some lung removed, not a leg.
We walk while we can walk.
So anyway, these nodules have always been present bilaterally, but you can only operate on one lung at a time (something about needing to be able to breathe...).
So after that surgery, I hopped back on a round of chemo but then had to go to Europe for a month.
I came back from Europe and did more chemo. But I also went to Iowa, Colorado, and South Dakota. I'll send pictures in my next email.
The chemo has had absolutely no effect on the lung nodules. They just keep growing. But thankfully, my lung surgeon is happy to go chop away.
So in 8 hours, I'll wake up and go to downtown Houston to have a left lung lobectomy. When the surgeon comes to say hi before they knock me out, I'm going to try to talk him into not taking the whole lobe. I like breathing. But he's also one of the best in the world, so I suppose I'll trust his judgment.
Assuming they do take the lobe, I assume the recovery time may be longer, perhaps a one or two-day stay in the hospital, but my goal is to beat 20 hours.
Every month I do a circulating tumor DNA blood test; it's a newish technology that can measure semi-accurately how much cancer is floating around in your blood.
In the past couple of years of monitoring, the number has slowly but definitively come down. The past two times have been the lowest. This suggests chemo is working overall, which is good.
So if all goes well, the hope is that number can possibly get to 0, but it's statistically and physiologically improbable. It is, however, a worthy endeavor.
Regardless of that and what the road looks like ahead, I hope to see you on the other side of this particular tunnel. And I promise I'll send some photos and a more comprehensive update in some days. As it happens, I've procrastinated in my writing of this, and I'm typing it on a cell phone in bed, but it seemed appropriate to update you, and I do love sending emails while incapacitated.
Some FAQs maybe.
Can you breathe okay? Yes. Breathing feels normal. I did some lung function tests prior to surgery 1. They said I have 120% normal lung function.
How long does it take to recover? - Based on the last one (which is not necessarily indicative of this upcoming surgery), I felt no pain after 3 days. The only pain I did feel felt like that brief stabbing sensation when you have a stitch in your side after running or something. It got progressively better every day, gone by day 3.
Will you be cured after this surgery? - No. Stage 4 cancer is like a felony. It doesn't go away. There is no curing it. Very, very rarely it can go away for a while.
What happens after the surgery? A few weeks of recovery and then back on the chemo wagon. Then some scans to see what is going on in the body and where, if anywhere, the cancer is remaining.
Are you scared/mad/nervous? Certainly none of those. I'm kind of excited. It's a waste to lament that which you can't control. Truly, I think this is all kind of fun, but I'm a droll fellow.
With that, I'll leave you for now and hope that this finds you well. There are maybe 10 to 15 of you that I keep updated on these matters, so cherish it. And don't tell anyone else. Mostly. It's a HIPAA violation.
See you on the other side.
Now ft. 20% less lung!
I've become more sophisticated and made an email group that makes it easier to send updates to.
And for posterity, I've also decided to keep these missives on the interweb.
(A repository of information of this ilk:
http://buffalochris.com/cancer
Obviously I'm picky about who I send these things to and don't tell most people much of anything, but you're a special lot. And if you do think of someone who would benefit from having this info, you can share it with them at your extreme discretion. Or tell me their email address and I'll consider adding them to the list.
To assuage your fears, I've not included anything about death in the title.
and the very nature of me sending this it should let you know in some way that I did not perish during or immediately after surgery, so that's a plus.
Primarily I write to say thanks for the support and replies and prayers and thoughts and love.
But while we're here, I may as well fill you in on the finer points of what happened and what's probably next and whatever.
Quick backstory on the procedure and required tubing-
Cancer floats around and takes up residence where it likes. In my case it moved to the lungs, primarily the right middle lobe and one small location on the left lung. It's pretty common in Stage IV.
I went in for a middle right lobectomy, which is where they take out a whole lobe of your right lung. Right lung has 3 lobes, left has 2 because the heart takes up some space and there's only room for two.
The surgery is a robotic assisted one (Da Vinci Xi) as opposed to cutting a huge space between your ribs and doing an "open" surgery. The robot makes 5 holes, the surgeon operates the controls of the robot.
Before they do anything, they have to put a tube and a camera down your trachea. They use the camera to guide the tube to the correct lung and then the tube seals off the lung (in this case my right lung) so that it can be operated on. Left lung is left to do the breathing.
They do the surgery, super glue you shut, and kick you out to the hospital floor.
The main complication is a collapsed lung/ pneumothorax since they made a bunch of holes in the chest wall and the lung itself may leak after the surgery. External air in the chest is a bad deal.
To let the lung heal and prevent this lung collapse, they stuck a huge tube in you which prevents air from filling in the pleural space. This is called a chest tube. It's literally a huge tube that goes through your ribs and ensures your lungs live in a vacuum
The Surgery
April 2 2024, 0900 my parents and alleged sister and I went to the cardiothoracic surgery floor of the hospital. They waited around, though I told them it was unnecessary, and I sat in the pre op area, had some X-rays done preop, waited around, put on a hairnet, and waited for the surgery team to be ready.
Not sure why I had to wear the hairnet. I asked if I could skip it...but they told me it was best to wear it. I don't think "they" really know why though.
Anyway, the surgeon stopped in before the procedure and we talked about nothing. I didn't have any questions and I was fine just hanging out, even though they didn't give me sedatives or hard drugs at all.
Rolled into the operating room about 2 or 3pm or so. I made sure to tell the anesthesiologists to be liberal with the illicit drugs since I don't get the opportunity to dabble in Propofol often. They obliged, I think. Because I was told to take a deep breath and then don't remember anything else.
Propofol, Versed, and some good old fashioned fentanyl kept me out until recovery. I was curious how long things took so my first question in my semi-conscious narcotic haze was "what time is it?"
730pm.
They wheeled me to where I was staying. Family came in, they left and went home. I spammed the pain medication distribution system.
It's set to only give you one dose every 10 min; in this case another opioid called Dilaudid or Hydromorphone.
The following morning when they checked the machine they noted that I had dispensed medication some normal number of times, maybe 16 or so, but that I had pressed the button 360 times.
I dont't recall it being particularly painful but on the spectrum of midevil torture - dayspa, it's somewhere in the middle.
In the morning the Dr's staff came in and began slowly taking things down or removing misc. tubes and lines. Nerve blocks, arterial lines, IVs all got removed little by little. Early afternoon the staff came back in and pulled out the chest tube after being happy with what they saw in x-rays.
I knew of the chest tube going into the surgery so I was generally prepared mentally. There's still something weird about people yanking what is essentially the size of a garden hose out of your ribs. It only feels weird for a second , they put a single stitch in to keep things sealed up, and then you're good.
Being untethered, I felt compelled to walk around. Sit. Eat my hospital food.
Did a final Xray in the afternoon and then was discharged about 2pm. Dad and Jennifer waited around for me to get the final paperwork and I eventually walked out of the hospital about 5pm.
The hospital staff really hates it when you walk out. They want to call a whole "transportation" team and have you in a wheelchair, etc. I tried to reason with them at the desk, but they didn't see it my way and told me to wait for the wheelchair. I told them "I'm gonna go down the elevator now" and I went. They yelled at some staffer to follow me. He was cool. I think he was secretly happy that he got to go on a side quest.
I never took the pain meds they sent to the pharmacy, and breathing got easier each day to the point where now, 11 days later, I feel 100% normal aside from feeling like i got stabbed in the ribs 5 times 10 days ago and the wounds are healing. They're not so painful though.
What's Next
I have a follow up with the surgeon in a week or two or something. I assume we'll schedule the 2nd lung surgery at that point and go over the results from this surgery. Overall it seems to have gone fairly well.
There are multiple possible paths but i think what probably happens is:
Schedule 2nd lung surgery, get it done ASAP (early May possibly), recover, and do clean up chemo for a bit. Have some scans. Do some tests, see what is left and where it is and how it can be treated.
If not a quick surgery window, hop back on chemo to nuke the cancer cells that are left and then do surgery in the Summertime. Imaging. See what's left. Chemo.
Something like that.
Again, this is not a thing you "cure" but in some rarer instances it can be treated to the point where it goes away for a while.
In any event, it's an interesting road with lots of cool characters in it and people I never would have met otherwise and I actually quite enjoy it. I don't recommend you do the same thing I did, but it's far from bad, and I'm reminded repeatedly from the little signs in the world that I am the benefactor of the amazing advances of modern medicine as well as an untold series of miracles small and large; from seeing magic on the molecular scale to experiencing the grandiose sense of splendor in the ephemeral electrons that equate to the essence of cosmic existence itself, life is pretty cool.
I need to finish the Bronco, though....
Onwards.
-C
Updates from beyond the grave (kind of)
Greetings subscribers/people I forcibly email,
I have updates.
Apparently when you blind carbon copy a bunch of people you can't just reply all and keep the thread going so I have attached the prior update below for your edification and perusal. But here's the latest:
I write to you on this eventide just hours prior to having the middle line of my right lung removed.
I have leveraged technology to schedule-send this email while I'm otherwise incapacitated and on the operating table. Hopefully not dead, but most certainly intubated and unconscious on a stainless steel mesa, most probably lingering in an anesthesia induced blackness before I bounce back to the reality of a PACU. So that's pretty cool.
When we last left off I was sipping wine on a high speed train to London in late August 2024.
When I got back from that trip I promptly started chemo; a cocktail of drugs administered via a central line that goes straight to my heart, which is pretty cool.
This era's flavor was:
cetauximab, oxaliplatin, capcitabine.
The cetauximab is actually an immunotherapy, and apparently the professionals say that immunotherapies aren't chemotherapies. All tastes the same to me though.
Cetauximab is notorious for creating a rash on the skin. Allegedly the worse the rash the better it works....so by that standard I should have been completely cured and reverse aged to like 18 because the rash was terrible.
However...it didn't stop me from doing things.
September I spent watching Aggie football in College Station and then in the latter 3 weeks of the month I went on an epic 3 week road trip to Canada by way of the nationally historic Yellowstone Lodge. Saw a mountain lion, grizzly bears, snow, bison, moose, etc. 10/10
In Early October I flew up to Rapid City South Dakota for a week of drone work looking at the Black Hills of SD and Wyoming.
Late October I saw Dashboard Confessional (which is a band, for all the olds) in Houston and then flew to Maine to spend spooky season in the cabin.
I got back in Early November just in time to head to San Diego for a work trip which was great. Weather was fantastic, people had a nice time.
Late November dad and I went to South Padre to see a rocket launch, I went to Ren faire (don't recommend), family came to visit for thanksgiving and we got a Christmas tree,
And in early December I decided I would start tearing apart the kitchen for a "light" remodel.
(Side note...bought the little stuffed pumpkin in London and it's become a weird travel buddy)
Somewhere around November or December between all of these activities and chemo every two weeks, I had another CT scan (or maybe it was a PET scan with the radioactive sugar, they all blur together)
Prior to the chemo the last imaging showed some suspicious spots in the abdomen and on the liver in addition to some new lung nodules
The results from this scan in Decemberish showed no suspicious activity in the abdomen. No unusual activity in the liver, but the lung nodules got a little larger and a little more numerous. Overall decent news...except for the lung thing.
So I had a conversation with the doctor. Her plan was chemo for life. Which is a pretty standard route ...and is exactly how it sounds.
I told her I wanted to be aggressive about the treatment, chemo for life is lame and old and generally ineffective at treating the lungs
I asked about other options for treating the lungs and she said she could look in to it.
She didn't sound super serious about looking into it. Or at least not at the level of expedience that I wanted so I went home and scheduled an appointment with the downtown Houston Medical center for a surgery consult.
It was the same hospital system I use in the Woodlands but just the main medical campus. So my existing Drs office !caught wind of that and all of a sudden my case was reviewed by the medical board, I had an appointment with the chief of thoracic surgery, and things got rolling.
Since the lung metastisis were growing we also changed the chemo combination which I was more than glad to do because the rash was brutal by this point.
In January or so the new recipe was/is ironitican, Fluorouracil, other vitamins and minerals that cancer hates. It's a pretty strong mix.
(Google:
FOLFIRI is a chemotherapy regimen used to treat advanced cancer. It is a combination of three drugs:
Fluorouracil (5-FU): An antimetabolite that interferes with DNA synthesis.
Leucovorin (folinic acid): A form of vitamin B9 that helps 5-FU work more effectively.
Irinotecan (CPT-11): A topoisomerase II inhibitor that damages DNA and prevents cancer cells from dividing. )
The first day of the treatment is rough...but overall I've handled all the chemos pretty well.
Jan/Feb/Mar I worked around the house, made progress on the kitchen, went to the rodeo a few times. I just got back a few days ago from another San Diego work trip that went really well, and now that surgery date has finally come.
Originally they wanted to do it at the end of March but I didn't want to miss the San Diego trip.
So initially they're going to place a camera down into my trachea and then seal off the right lung. Then they're going to go in with a robot, make 5 holes in my chest, remove the middle lobe of right lung. Then they seal everything up, turn the lung back on and see how everything works.
You have to have a chest tube so you don't get a pneumothorax and so they can see if the lung is leaking air...that sounds like the worst part.
But 2 day +/- hospital stay and then I'm back into the wild.
I did have to do some some preliminary lung volume tests...results came back at 122% capacity. Strong like bull.
And truly there are absolutely no signs or symptoms. No shortness of breath. No cough. Nothing.
There's no guarantees on this route but anecdotally I have heard first hand experiences of other patients in similar situations and after surgical removal of the lung mets, all signs of cancer can go down to undetectable levels.
After this surgery on the right lung i would have another on the left and then, in theory and in a perfect world there is a chance that all the cancer could be gone for a little while.
That's the hope. But anything that happens along the way is all part of the journey.
Aside from feeling awful on the first day of chemo, life goes on pretty well.
That's your update for now. See you on the other side.
An update. (Spoiler alert: I'm still not dead.)
Greetings subscribers/people I choose to email.
I know it's been some time since the surgery but until recently there was not much of a concrete update to give.
I lived after the surgery, obviously. I thought it was a 3 or 4 hour procedure so I was a bit shocked when I walked in and they told me just before going under that it would be 9 or more hours.
But on the plus side, I only had to sit with that anxiety for about 45 minutes before the anesthesiologists came in.
Woke up on the PACU and of all the possible outcomes of the surgery, the reality was the most favorable one. It could have been worse. The interdisciplinary team of surgeons seemed pleased.
Hospital stay itself was uneventful. I was walking around on day 1. Off pain medicine day 2. Sent home day 4/5 and I walked out of the front door on my own two feet. No wheel chair needed.
Over the entirety of May and most of June I dealt with infections which are common with the type of abdominal surgery I had. 3 or 4 rounds of oral and IV antibiotics got me better but it was a long slow annoying process.
The rest of the time in those two months was adjusting and recovering which is generally easy when you're not showing signs and symptoms of an infection. It was up and down. Sometimes fine. Sometimes more hearing excruciating.
By mid June I went to Galveston for fun, went to a Noah Kahan concert in the woodlands, worked on the bronco. In July the hurricane came through. No real issues except wind damage and some downed trees. I actually had a doctor's appointment at peak hurricane hour for my location and drove to the Drs office. It was a bit harrowing. Almost got blown off the road, but it was memorable, my appointment took place, and the drive home was uneventful.
In the later half of July I flew to Maine and spent time in the cabin. Rode e-bikes in Acadia, saw more bald eagles than I ever have up there. Drove to Canada, saw sunrise from Cadillac mountain, ate blueberries, etc etc etc.
(Lubec, Maine)
August 6th I caught a plane to London and I've been there since. I come back on the 22nd.
Eifel tower. Olympics closing ceremony. Train to Switzerland, Taylor Swift concert in Wembley, etc etc.
(8am walk ft pigeon)
So: 9 hour surgery was good. All surgical margins were negative for cancer meaning in theory nothing was left behind.
After some CT scans and an MRI in July there are some questions marks that indicate cancer is still active though.
So I had a followup PET scan where they Inject radioactive sugar in your blood. Cancer likes to eat lots of sugar, so the sugar goes in, cancer grabs it up, and those areas are temporarily radioactive so they light up on the CT scan. It's semi accurate but not infallible.
After the PET:
-3 new spots on the lungs (common area for the cancer to move to)
-maybe a new liver spot
-possibly a lymph node
Best outcome post surgery would have been "hey, we don't see anything, have a good life, we will rescan in 3 months"
But in this case it's "hey looks like there's some stuff going on still. So more chemo"
Chemo starts on the 26th when I get back.
They're adding a new drug this time, a monoclonal antibody that has pretty good efficacy in certain people.
So it's all the normal poison drugs plus this one.
To be honest I think my liver might be fine, I think the abdominal lymph nodes could be an anomaly, and I think the lung spots are legit.
Lung metastasis are usually slow to grow and easier to treat via cryo ablation or laproscopically, so that's a potential plus.
But if it's any testimate to how bothered I am about it, I'm writing this on a high speed train traveling in a tunnel deep under the english channel at 220mph from Paris to London while I drink French Syrah and have been walking 5-8 miles a day. I feel good.
The chemo is probably going to suck. First round back in always seems to, but usually gets better afterwards and life goes on.
Cancer cells are smart and build immunity to chemotherapies and evolve so it's an ever changing game until eventually you run out of treatment bullets.
Obviously the hope is that the new drug, cetauximab, works, there's a complete clinical respone, and all signs of cancer are undetectable for a time.
The statistics say that's possible, not probable. But those are good enough odds in these matters.
Two week cycles, 6-8 rounds. Scans in-between to see how it's working and if it's working.
After that, who knows? But that's the immediate future.
Or near future, rather.
The immediate future is this wine and a Taylor Swift concert tomorrow....
-C
Pre surgery update
Greetings friends and family and associates and stragglers.
Here's your update-
Jan went well overall, did radiation every day, minimal side effects. Did my last treatment on a Feb Monday morning then hopped on a plane to San Diego.
After that they give you an 8-12 week break for the radiation to keep working and then scan to see how things look and go from there.
Some slight confusion happened when I did my MRI about 8 days after the end of radiation instead of 8 weeks, so the results were not necessarily representative of the maximum effect of the radiation.
Insurance only gives you one MRI every 3 months, so I paid out of pocket and got that done this past Thursday. Had some meetings with a surgeon, talked about options.
It's been a little hypothetical and up for discussion/scheduling based on surgeon availability due to how complex the surgery might be. but as of Friday night it was confirmed:
Going to surgery tomorrow. Monday, April 29.
7am start time. 4ish hours, a few hours in recovery, could be back with the living Monday night or Tues AM. It's a robotic surgery in downtown Houston. 5 tiny incisions, the surgeon sits at the controls of the robot and manipulates the arm. They plan to make a couple of other incisions as needed, if needed.
Hospital recovery is 3-6 days, overall recovery 6-8 weeks if things are optimal. Slow downs and complications in healing are common due to the effects of radiation so if there are any snags, could take a year to fully heal.
But the goal is to remove all of the bad tissue and they think they can get it all.
After that I'm sure there's many follow up appointments, scans, etc.
Sometimes people do "clean up chemo" to knock out any remaining cells floating around. So that could be the next step.
I feel physically fine. Strong, normal, nothing out of the ordinary. The past 12 weeks pre-surgery but post radiation have been very normal and nice. Got a lot of work done on the Bronco. As it sits right now it's technically running and driving. Has steering and brakes and lights and everything. Will get it on the road as soon as possible after this little operation.
Parents are going to be there. I'm sure they'll get in touch regarding outcomes.
They're going to tell my friend Mattie when I'm out, and Mattie will reach out to some friends of mine and let them know.
Otherwise you can text and I'm hoping to be functional by Tuesday AM.
See you on the other side,
-C
Not dead yet.
Greetings friends,
Happy holidays, good tidings, cordial niceties, etc etc etc.
Thought it would be useful to give an update on the state of affairs specifically regarding health, starting at the top since I've been wrongly accused of not discussing such matters.
Sept 1 2022 - Diagnosed with stage 4 colon cancer. Stage 4 means it's spread to other organs, in my case the liver which is pretty common for this cancer.
Very generally, treatment approaches vary but go something like this:
Chemo to get the cancer to shrink or maybe go away. Chemo is systemic and works in the entire body
Radiation to shrink/kill the cancer even more. Radiation is targeted
Surgery - physical removal of the bad bits.
After the initial diagnosis I went through a few machines (CT, MRI, etc), got a liver biopsy which was not fun, and had a port installed which was pretty cool.
The port and biopsy were done at the same time with twilight sedation and fentanyl. So I remember the whole thing well but couldn't feel most of it.
The "port" is quick and easy access for IVs instead of having to stab a vein every time. Useful when doing lots of chemo treatments. The fish a tube down into your heart to mainline the drugs.
The liver biopsy came right after they put the port in (I think....i could be wrong though. I was on drugs) and they took a core sample with a huge needle. Even with the drugs, I still remember feeling that punch of the needle when they took a plug from my liver.
They needed to sample to prove the cancer had indeed spread but it was mostly semantics given the CT and MRI imaging. Biopsy came back confirming it was cancer. No surprise. With the new port installed, I was prepped for chemo.
Oct-March 2023 - Chemo.
There's "Lines" of treatment when it comes to chemo. 1st line- the basic stuff that usually works. 2nd line- alternatives that may be less effective overall but could work. 3rd line- basically a hail mary.
Initially I was anemic, so they injected me with a few bags or iron over the course of a month. Apparently you need red blood cells...
After the blood work was good, I started on a cocktail of the basics.
5-Fluorouracil - Basic chemo drug. There are two forms - You can eat it in pill form (which is what I did this round) or have a tiny football sized pump you stay connected to for 48hrs
Oxaliplatin - has actual platinum in it. Has some serious side effects, namely cold sensitivity and peripheral neuropathy.
Avastin - Cuts off blood supply to quickly growing cells. Also can hurt your kidneys and make your blood pressure skyrocket.
Each "cycle" was a total of 3 weeks. Go in on day one, get hooked up to a bunch of drugs on an IV pole, take the pills 2x a day for 14 days, and then take a week off. Rinse, repeat. I ended up doing 9 cycles, I think.
CT scans showed a good response. the primary tumor shrank, as did the liver ones.
So the focus shifted to fixing the liver. Initially, the place I started treatment thought they would implant some radioactive spheres in the liver tumors to kill them. Then they called me one day and said "No, we're gonna keep you on chemo."
At that point I started looking for a 2nd opinion and by sheer good fortune, stumbled into St. Luke's. They were actually recommended by a nurse from a competing hospital.
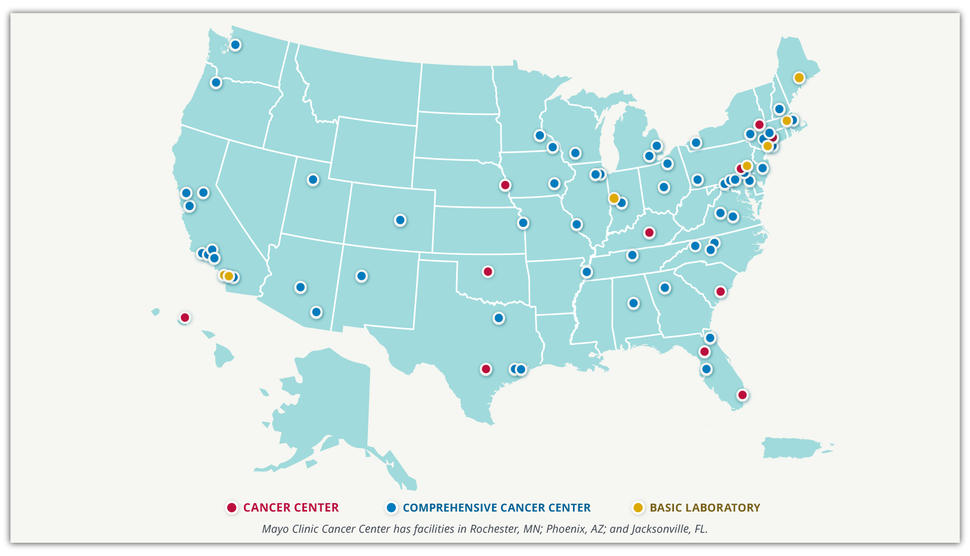
Note for context- Stage 4 cancer isn't typically a treat-and-you're-cured deal. Even if it does go away completely (which is rare) it usually comes back. It's like medical whack-a-mole. Some are on chemo for life and never get surgery. I felt like the original doctors were phoning it in. When meeting with the doctor at St. Lukes, it was the first time I heard a medical professional use the word "cure" and even though I know those are long odds (and you should know too those are very, very long odds). I appreciated the intent. So I changed hospitals.
There are not many NCI-designated hospitals in the country, but this new one happens to be one of two in Houston (the other one being MD Anderson).
By the end of this little block of chemo my Blood pressure was so high I had to get on medication for blood pressure. 170/110, at one point. The avastin is known to do it. Avastin also makes you susceptible to bleeding. After talking to surgeons and having my case looked at by a board of doctors, the next major step was liver surgery.
March - July 2023- Heal from the chemo.
Finished the chemo. The avastin has to be long gone before they'll do surgery. So I had some scans, and then I went to girl scout camp and I met with the liver surgeon a couple times. Surgery date was planned for August 2nd I think.
Surgeon seemed pretty confident they could get the job done (not sure why the first dr ruled out the possibility of surgery) but did mention there were two routes to go- robotically through small incisions, but that may make it harder and could leave some bad tissue behind, or an open surgery which makes it easier to work. I told him something directly along the lines of "If we're doing this, just open me up."
August 2023- Liver chopping
Had the first surgery of the day. generally went fine.I woke up some 5 hrs later with 40% less liver but the surgeon seemed pleased. Left the hospital 3 days later. And when I told them to open me up...they certainly did. Got a cool scar that looks like a mercedes benz logo. They put a temporary tube in to drain my abdomen as it healed. Long story short- that tube was touching the nerve that activates the diaphragm. So for 3 days I couldn't take a deep breath to save my life. But as soon as they pulled out 3 ft of tubing...I was instantly healed. Overall it was pretty painful. They have that thing where you hit a button and it shoots you with some morphine or whatever...the nurses came in one morning to check and make their notes and whatever and casually remarked to each other that over the course of the night, I had hit the button some 150 times and been successfully administered the medicine about 20 times (it's on a time delay). I got good at setting my internal clock to the pain medicine clock though.
For the rest of august I took drugs and laid in bed mostly. Cool fact- I didn't get staples. They closed the wound with sutures and then for 3 days in the hospital, it was covered with a negative pressure dressing. Two little hockey puck sized pumps kept a vacuum on the incision site meaning no staples were needed.
Sept 2023- Biopsy results and imaging
Surgeon felt good, but the biopsy results came back questionable. The idea is to cut out the bad stuff with a buffer zone of healthy tissue around it. A margin, as it's called in the business. If you cut a tumor out and the margin is negative for cancer, then that's good. If you cut it out and the margin has cancer cells...then there's prob still cancer cells in the liver.
Biopsy said there were some inconclusive margins for one or two of the removals. I think there were 5 tumors total, one was deep and got microwaved. The others got cut out and removed. Overall they said they took about 40% of the liver out.
CT and MRI scans showed that overall the cancer had grown (but that makes sense, because I was off chemo for 4 months) and that the liver looked okay.
Oct-Nov 2023 Chemo part 2
This time the cocktail was 5FU (the pump version), Oxaliplatin, and Irinotecan.
Widely regarded as the most aggressive and strongest blend of drugs there is. Sometimes avastin is added, but it wasn't in my case.
Did 6 rounds of this, each round 2 weeks instead of 3.
Day 1 - go in, sit for 6 hours, get injected with all the drugs. Have the football pump hooked up to port, go home.
Day 3- Come back in to have them remove the pump and inject me with a needle that allegedly tells my body to make white blood cells (those get killed by the chemo a lot)
Day 4-13 - live
Day 14 - repeat
The first 3 or 4 treatments were accompanied with pretty awful nausea, but I bounced back quicker after each treatment. Last chemo of this episode was Nov 27
Dec - Scans, Chemo-Radiation
Scans following the strong chemo cocktail were...okay. There were no changes in the liver, which is good given the margins were originally suspect. Parts of the primary tumor shrank, and some lymph nodes shrank a tiny tiny bit.
Met with the radiation people and after some initial confusion about what they were treating (secondary liver tumors or the main primary tumor) I went through the process of getting set up to be shot with radiation to treat the primary tumor (liver looked good in scans, no need to radiate).
They vacuum-form a little mattress to your body to make sure you're in the exact same place every time.
The plan is long course external beam radiation which is like...28 treatments or so. Every day, except weekends and holidays. On radiation days I also take chemo pills.
First session was this past Wednesday. It takes about 15 minutes. I lay on a table, a machine spins in a slow circle and shoots beams at me.
Side Effects like nausea, fatigue, etc are cumulative. they say you don't notice til week 3ish or so.
Last session is Feb 5th. So far so good.
Feb 2024 and beyond
After radiation there will be more scans, and then a few things could happen.
1- Scans look good, have surgery to remove primary tumor.
2- Scans show no change - more chemo or diff drugs, maybe
3- Scans show total response, no more tumor visible - carry on with life. get scans every 3 months to see if anything comes back. go from there.
So far I feel like it's working after 3 treatments. We'll see how it goes.
There was one instance in November where I had to do Chemo on a monday instead of being in San Diego. I was able to get to San Diego on Tuesday, though. Aside from that one day none of this has stopped me from doing anything I otherwise would do, or wanted to do.
And though impossible to believe for some, I'm not sad or depressed or mad or upset about it. Mostly I think it's kind of funny but I have a weird sense of humor.
Overall I've learned that the treatment is an inexact science and reactionary based on results, so when people ask me what's next and I say "I don't know..." it's because I really don't know. But generally the roadmap is above.
I think that's everything for now.
See you in 2024.
-C